Why in the News?
The World Health Organization (WHO) released the Global Antibiotic Resistance Surveillance Report 2025.
Key Findings of the Report
- Antibiotic Resistance: In 2023, approximately 1 in 6 bacterial infections worldwide was caused by antibiotic-resistant bacteria.
- Antibiotic Resistance rose in more than 40% of the bacteria-drug combinations tracked between 2018 and 2023.
- Gram-negative bacteria pose a severe threat.These are pathogens that are hard to kill and resistant to multiple drugs. E.g., Escherichia coli (E.coli)
- Regional Hotspots: AMR was most frequent in Southeast Asia and the Eastern Mediterranean.
- India Related Finding: Around 41% of bloodstream infection reports came from China, India, and Pakistan combined.
- Improvement in Surveillance: Country participation in the WHO's Global Antimicrobial Resistance and Use Surveillance System (GLASS) has increased four-fold since 2016.
- GLAAS (2015) is a comprehensive global system designed to monitor antimicrobial resistance and support appropriate use of antibiotics worldwide.
What is meant by Antimicrobial Resistance (AMR)?
- AMR occurs when bacteria, viruses, fungi, and parasites evolve to withstand the drugs designed to kill them.
- Strains of bacteria, viruses, parasites, and fungi that are resistant to most antimicrobials are called Superbugs.
- Due to drug resistance, antimicrobial medicines become ineffective, and infections become difficult or impossible to treat. E.g., Multi-Drug-Resistant Tuberculosis (MDR-TB)
- This increases the risk of disease spread, severe illness, disability, and death.
- AMR is a natural process that happens over time through genetic changes in pathogens.
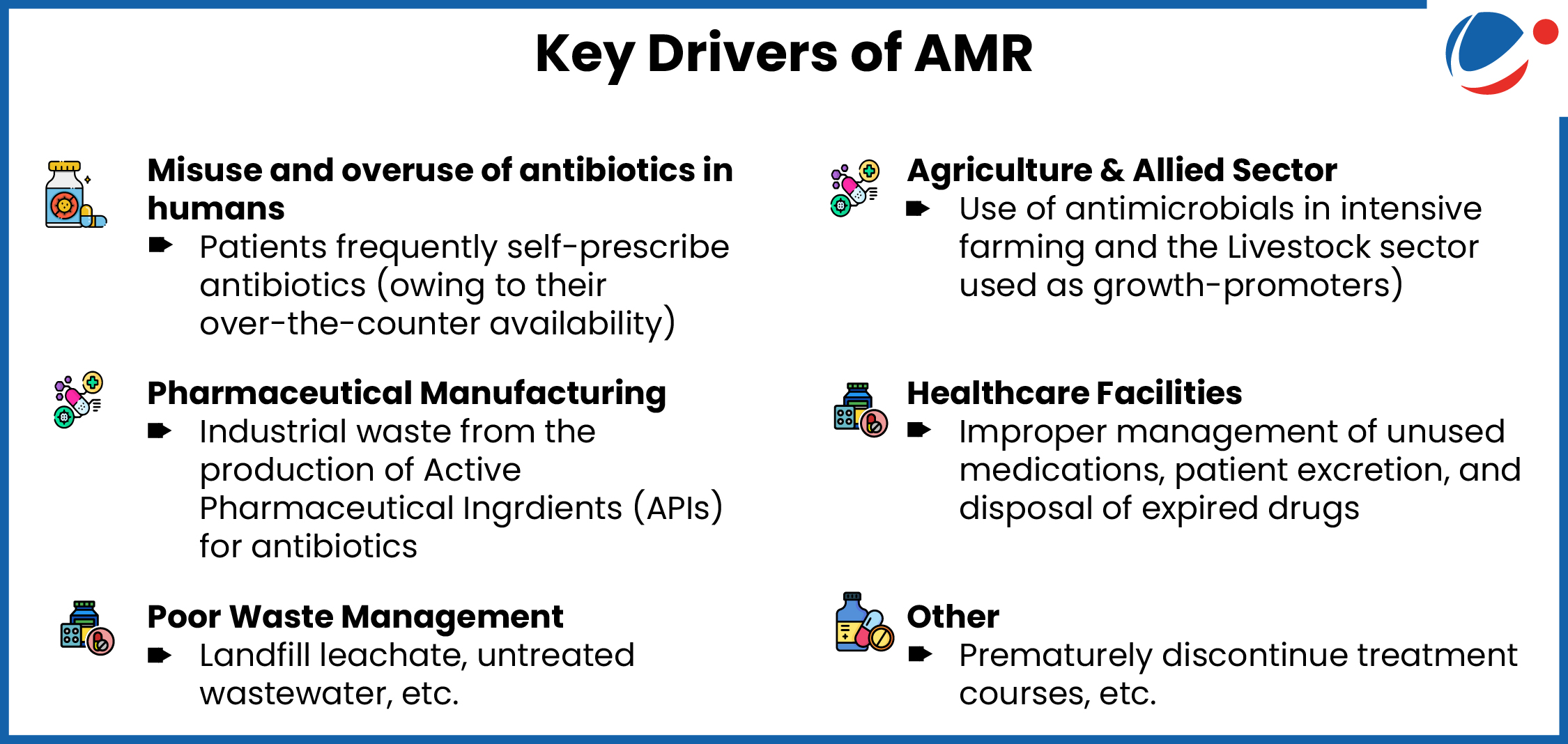
- However, its emergence and spread are accelerated due to several anthropogenic factors.
- WHO recognized AMR as one of the top ten global health threats.
- It is often described as a silent pandemic.
Why is AMR a Global Health Threat?
- Mortality and Morbidity: Bacterial AMR was directly responsible for 1.27 million deaths in 2019 and contributed to nearly five million deaths globally.
- Economic Impact: Resistant infections could cause an estimated $3 trillion in global GDP losses per year by 2030.
- Outpacing advances in modern medicine: It makes infections increasingly difficult to treat and renders medical procedures such as surgery far riskier.
- Threat to Food Security: Drug-resistant infections impact the health of animals and plants, reducing productivity in farms.
 Measures taken to address AMRNational
Global
|
Way Forward
- Implement integrated intervention packages: It includes infection prevention and control, water, sanitation and hygiene, vaccination, antimicrobial stewardship, and strengthening of the laboratory.
- Antimicrobial stewardship aims to educate and support healthcare professionals to follow evidence-based guidelines for prescribing and administering antimicrobials.
- Strict implementations of Drugs and Cosmetics Rules, 1945: All pharmacist associations shall adhere to the rules and sell antibiotics only with valid prescriptions.
- Enhancing Monitoring: Generating reliable surveillance data, especially from underserved areas.
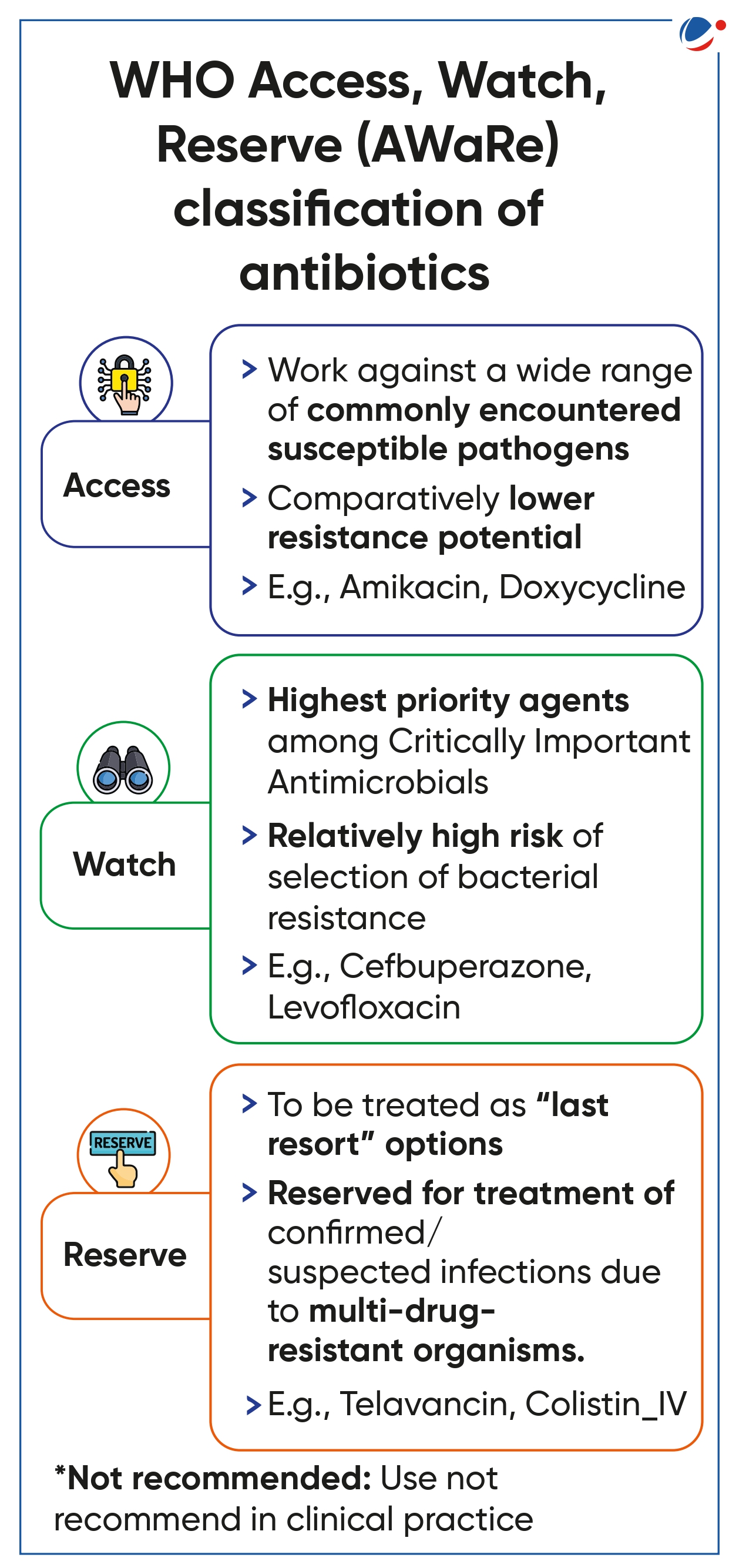
- Appropriate Antibiotic selection: Reduce use of AWaRe Watch antibiotics and increase the use of Access antibiotics
- Other: Enforce stricter controls on antibiotic use in Agriculture and Veterinary.
- Expand social protection, such as Universal health coverage (UHC).
Conclusion
AMR poses a grave threat to global health, food security, and sustainable development. Combating it requires a coordinated One Health approach that integrates human, animal, and environmental health efforts. Strengthened surveillance, rational antibiotic use, and global cooperation are essential to preserve the effectiveness of existing antimicrobials and safeguard future generations.