Why in the News?
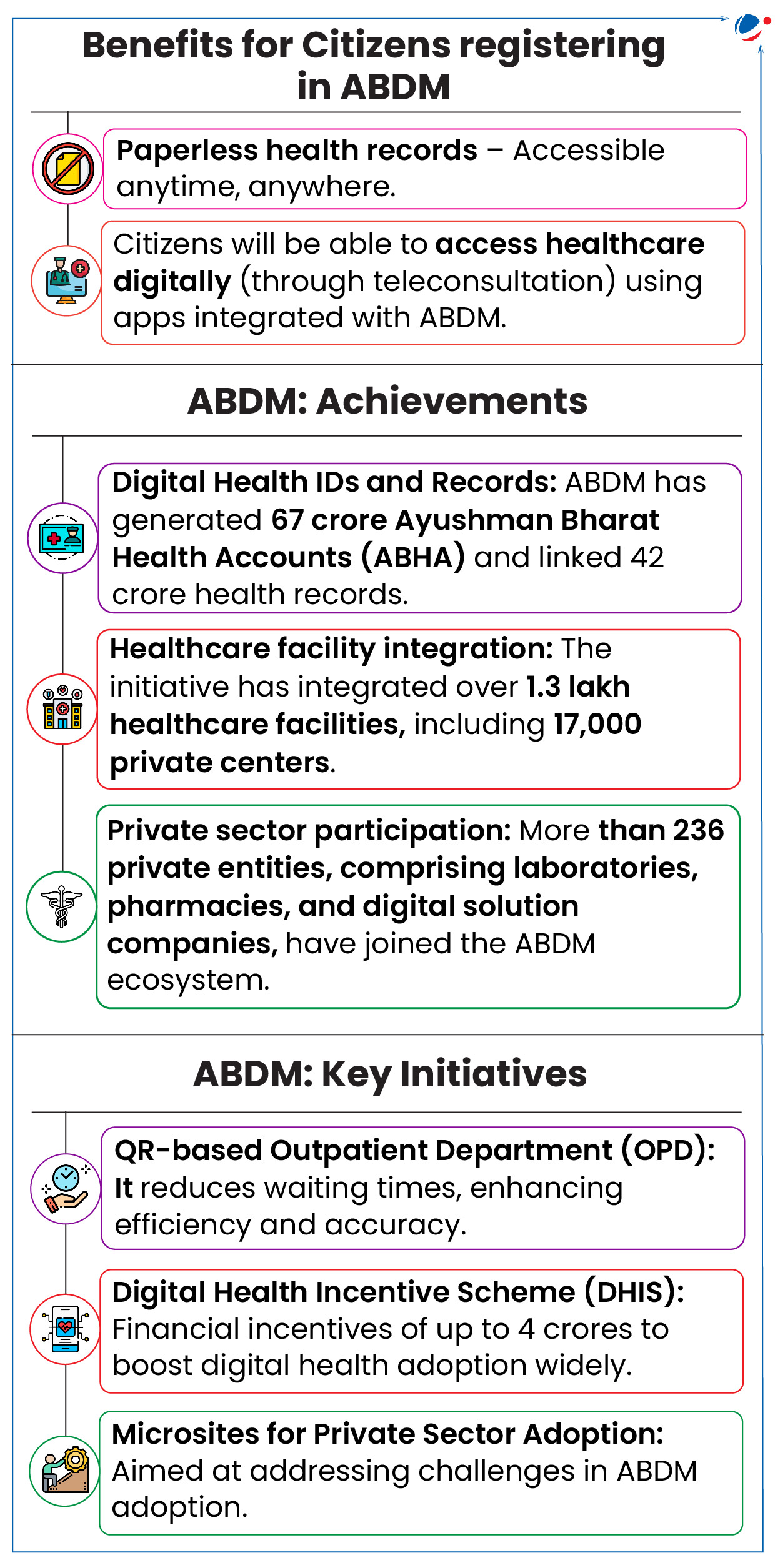
Ayushman Bharat Digital Mission (ABDM), launched in 2021, marks three-year towards enabling Digital Health.
About Ayushman Bharat Digital Mission (ABDM)
- ABDM aims to connect the digital health solutions of hospitals across the country.
- ABDM, as a 'Digital Ecosystem', will also enable a host of other facilities like digital consultation, consent of patients, etc.
- Key Principles: Inclusivity; Free of Cost Registration; Opting out of the ABDM Ecosystem as per one's will; single source of truth with no other parallel copies of one's medical records; Federated structure to ensure privacy; Voluntary Participation.
- Implementing agency: The National Health Authority, an attached office of Union Ministry of Health & Family Welfare.
- Components of ABDM Architecture
- Ayushman Bharat Health Account (ABHA) ID: A unique 14-digit number to store and manage health records.
- Healthcare Professionals Registry (HPR): A unified repository of healthcare professionals across all medicine.
- Health Facility Registries (HFR): Repository of health facilities of the nation (both public and private).
- Health Information Exchange and Consent Manager (HIE-CM): To ensure that data exchange is driven by informed consent.
- Unified Health Interface (UHI): To Facilitate the discovery and delivery of health services.
- National Health Claims Exchange (HCX): To standardize the insurance payment ecosystem.
About Digital Health
- The WHO defines digital health as the "field of knowledge and practice associated with the development and use of digital technologies to improve health." It includes:
- Digital health applications: Electronic Health Records; Telemedicine; Wearable Devices to monitors health aspects; and Health Information Systems for managing, storing, and exchanging health information.
- Digital health technologies: AI and Big Data to quickly identify patterns in tremendous volumes of data; Internet of Medical Things (interconnected medical devices); Augmented Reality to make medical procedure more efficient; Digital Genomics, etc.
Significance of promoting Digital Health
- Seamless medical record sharing: Enables Indians to use IT-enabled tools to share prescriptions, blood test reports and X-ray diagnostics with doctors.
- Unique personalised medical account: Creates a unique health ID for every citizen and digital registry to facilitate seamless interactions between healthcare experts.
- Chronic disease management: Helps manage chronic diseases which have become a critical public health challenge in the past 15 years.
- Also, improve public health monitoring and advance evidence-based policymaking in the long run.
- Enhanced treatment for critically ill patients: Data portability could expedite treatment of critically ill patients, especially those suffering from multiple ailments.
- Comprehensive medical history repository: Creates repository alerting doctors to patient's medical history with one click, important for treating patients with comorbidities as highlighted during Covid-19.
- Also, gives patients options to choose which records they want to share with healthcare providers.
- This ecosystem will ensure old medical records are not lost as every record will be stored digitally.
Concerns pertaining to Digital Health
- Privacy and security issues: Unauthorized data access and breaches can compromise patient privacy and lead to identity theft.
- E.g., Personalized data collected can be exploited by insurance companies and pharmaceutical firms for targeted advertisement.
- Algorithmic bias: Technologies such as AI can result in unfair or discriminatory treatment. E.g., might lead to racial & ethnic disparity in healthcare.
- Equity and access issues: Unequal access to digital health technologies and digital literacy skills can exclude vulnerable populations.
- E.g., Poor internet connectivity in rural areas can make data entry and utilization of digital healthcare services a challenge.
- Lack of trust in digital healthcare systems: E.g., The failure of the UK's National Health Service digital system highlights the importance of earning the trust of healthcare providers.
- Lack of standardization in digital Cards: India struggles to standardize coverage and quality of existing digital cards (e.g., One Nation One Ration card, PM-JAY card, Aadhaar card, etc.), leading to data migration and transfer issues, as well as concerns over data security.
- Communication challenges in diverse healthcare ecosystems: Due to its linguistic and cultural diversity in India.
Way Forward
- Enhance universal reach: Ensure the Intelligent Health Solution is evaluated across a diverse user base, including displaced populations and diverse racial/cultural backgrounds, to improve quality of life and collaborative decision-making.
- Strengthen technical proficiency: Improve digital skills among medical teachers and students to better leverage digital health tools.
- Enhance targeted solutions: Create customized and individualized approaches to digital health tools, supported by empirical evidence.
- Build ethical oversight: A formal governance body can be established to develop frameworks for data collection, sharing, and usage and draft a "code of ethics".





